Introduction

Having access to fresh, healthy blood products is essential for many researchers working in a wide range of scientific disciplines, from immunology and genetics to pharmacology and toxicology. This can be a challenge and those who work in the field often struggle to find samples that meet their needs, leaving them with suboptimal samples that limit the accuracy and reliability of their data.
In this blog, we explore why fresh blood products are essential to many applications and look at the options available to source healthy blood products that meet your needs.
We will discuss:
• The different types of healthy blood products available
• The importance of using fresh blood for research
• Selecting the best source of blood products for your research
• National and regional public collection services
• Donation from within your organisation
• Commercial specialists in blood collection
• Securing the right source of fresh blood products for your needs
The different types of healthy blood products available
The type of blood product you should choose will be heavily influenced by the goal of your research and design of your study.
We have outlined the types of healthy blood products available in the table:
Blood product |
Collection method |
Application examples |
|
Whole blood |
Anti-coagulant tubes or bags |
Wide ranging: • Development and validation of diagnostic devices • Blood chemistry studies • Inflammatory and immunity research |
|
Leukopaks |
Concentrated leukocytes isolated by apheresis |
Highly concentrated nucleated cells from a single donor can be useful for large scale experiments, immunology research and immunotherapies e.g. CAR-T |
|
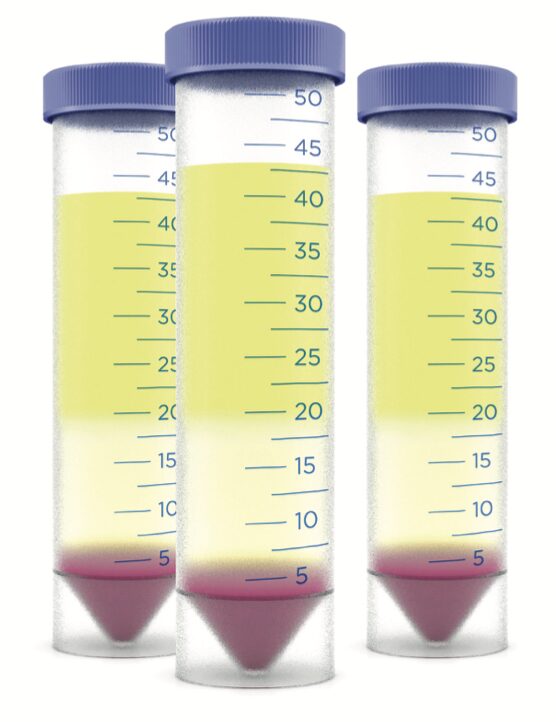
Peripheral blood mononuclear cells (PBMC) |
Centrifugation of whole blood, leukopaks or buffy coat over Ficoll-Paque density gradient media |
• Immunology and immunotherapies e.g., CAR-T • Cell therapy |
|
Buffy coat |
Centrifugation of anti-coagulated whole blood and removal of erythrocytes and plasma, leaving most of the white blood cells and platelets |
A rich source of PBMC and other white blood cells, which can be used in a wide range of applications |
|
Leukocyte reduction cones |
Leukocytes are isolated using an in-line filtration device during blood/platelet collection |
A rich source of PBMC and other white blood cells. Widely used to isolate total leukocyte populations for functional assays on cell types of interest in disease |
|
Plasma |
Centrifugation of anticoagulated whole blood |
Essentially serum with fibrinogen, however plasma may contain residual anti-coagulant which may affect assay performance. Widely used in bioanalytical and toxicology studies |
|
Serum |
Produced from whole blood collected in clot- activating tubes or in bags using the off-the-clot method |
Serum provides a highly representative matrix, but the clotting process will lead to the presence of factors that may affect assay performance. Widely used in cell cultivation |
|
Red blood cells (RBC) |
Centrifugation of whole blood |
Haematology research into conditions such as sickle cell anaemia, malaria and toxin exposure. Leuko-reduced RBC can also be used for research into leukotropic viruses, such as EBV and CMV |
|
Isolated cells |
Purified from leukopaks via negative immunomagnetic separation |
Wide range of applications including immunotherapy, CAR-T and immuno-toxicity studies |
The importance of using fresh blood for research
Cell functions can change rapidly following venepuncture, meaning that any delay in processing or delivery can affect how accurate the samples represent the in vivo environment, assay performance and any data that is generated.
The importance of fresh samples has been demonstrated in two particularly noteworthy clinical advances.
The first is liquid biopsies. In 2016, the FDA approved the Cobas® EGFR mutation liquid biopsy test for detecting lung cancer. This safe, non-invasive and easily repeated test provided patients with an improved diagnosis experience compared with traditional tissue biopsies.1
The second, CAR-T therapy, has the potential to revolutionise cancer treatment and involves modifying T-cells to produce chimeric antigen receptors on their surface.
In both examples, fresh healthy blood products were essential for generating relevant results that deliver true biological insights and advances.
How fresh is fresh for blood products?
According to the International Society for Biological and Environmental Repositories (ISBER) best practices guide, blood samples should be processed and stored within 1 to 24 hours of draw, depending on the analytical endpoint. After this time, the cell functionality starts to decline, which could have substantial implications depending on your application.
The importance of following best practices when processing fresh blood products
Following best practices for blood processing is essential
to minimise any potential changes to cell functionality. For example, research has shown that an increase in processing time after venepuncture from 8 to 24 hours resulted in about an 8% and 32% decrease in PBMC viability and cell recovery respectively, with the greatest impact seen on T-cell functionality, where a 36-56% loss in interferon gamma frequencies was observed. 3
In addition, platelets in plasma can easily degrade if samples are not handled correctly. This can result in platelet activation, which can contaminate samples and result in inaccurate measurements. 4
Given the potential consequences of delaying processing following venepuncture, a number of studies suggest that processing of products should be carried out as soon as possible following blood draw. 5-7

Selecting the best source of blood products for your research
In order to select a source of fresh blood products, you first need to assess which option will best suit the needs of your research. In general, there are three main sources of healthy blood products; national public blood collection services, specialist commercial suppliers and internal volunteers within your organisation. When reviewing these options, it’s important to consider:
- Supply timelines & consistency
- Donor characteristics & lifestyle
- Ethical & consent requirements
- Blood product formats available
- Collection & processing methods
Key questions to keep in mind when selecting a source of blood products
Collection & processing methods
Can the supplier provide details of how blood products are collected and processed?
Can the supplier adhere to specific collection and processing requirements that you outline?
What is required to ensure processes are consistent and ethically viable?
Supply timelines & consistency
How fresh do you need blood products to be?
Do you have a strict experiment timeline that needs to be kept?
Will the supply option be able to deliver consistently and within the timeframe you require?
Donor characteristics & lifestyle
Does your study require blood products from donors with specified characteristics e.g. sex, age, ethnicity, BMI?
Do you require donors who have not taken medication that may interfere with your research?
Can the supply option provide products that match specific characteristics?
Blood product formats available
Which blood product format do you require and can the supply option provide this?
Can the supply option consistently deliver the volumes you require?
Can the supply option continue to meet your requirements should you need to scale-up your research?
Donor characteristics & lifestyle
Does your study require blood products from donors with specified characteristics e.g. sex, age, ethnicity, BMI?
Do you require donors who have not taken medication that may interfere with your research?
Can the supply option provide products that match specific characteristics?
National and regional public collection services
Across Europe, there are a variety of public voluntary donation services which collect and supply blood, organs, and tissues for transplantation. When blood is unable to be used for clinical purposes, it can then be released to research organisations for non-clinical uses.
Supply times and consistency
The primary focus of these organisations is to supply blood and organs for clinical use, therefore they cannot guarantee a steady supply of blood products for research. Availability and consistency of fresh blood products is likely to fluctuate with clinical demand, which can impact research project timelines.
Blood product formats
Formats available
Voluntary donation services provide a multitude of blood samples, from whole blood and derivatives to leukocyte cones, which are produced as a by-product of plasma or platelet donation. Whilst most donation labs have the resources available to process these samples, supplying these products for research purposes is not the primary focus and therefore labs cannot guarantee freshness or a specific delivery window. This is something to consider if control over freshness and delivery timeframe is key to your research.
Collection device flexibility
Additionally, as the primary goal is to collect blood for transfusions, specific devices are used for the collection. Therefore, there is little to no flexibility on collection vessels, anti-coagulants, or how the blood is processed. For some research applications, having little control or consistency over these factors could have a detrimental effect on assay results and should be considered when choosing a source of blood products.
Donor characteristics and lifestyle
Pre-selecting specific criteria
Due to the nature of the service, public donation organisations cannot control or limit donor characteristics, as their priority is
to ensure there are enough donations to meet clinical needs. Therefore, researchers looking to use this service to source fresh blood are unable to pre-select donor characteristics that are of interest to their study. This can include age, BMI and blood group, which is something to consider if this is crucial to your research.
Medical history and medication
Similarly, there is no specific exclusion criteria for donors based on medical history or medication, therefore donors may be taking commonly used medicines, such as ibuprofen or other anti- inflammatory drugs. This may impact researchers conducting immunological assays, which could be affected by such drugs or their metabolites.
Collection and processing methods
Infection screening
It is imperative that donated blood for transfusions is disease- free, however clinical-grade screening for viral infectious diseases can be a slow process. To ensure freshness, blood used for research normally arrives at the receiving lab before testing is completed. It is therefore possible that the presence of infection is only recognised after assays have been run, resulting in the need to repeat experiments and posing safety risks for those working with the blood products.
Protocol flexibility
A final consideration for national volunteer donation services is the limited control you have over blood collection and processing procedures. This may require you to change the design of your study to accommodate the format, consistency, and quality of the products you receive.
Donor recall
Finally, donated blood and components are commonly anonymised with no systems in place to recall the same donor
to donate again. Depending on your research application, this might not impact you, but if your experiments require you to perform replicates using samples from the same donor, sourcing through a public donation organisation might make this an impossible task.
Ethical and consent requirements
Typically, volunteers who donate at public collection services give consent for their blood to be used for non-clinical uses. As a result, donors do not provide specific consent for their donation to be used in genetic and commercial research, or waive
their IP rights. Depending on your organisation and research applications, you might need to confirm with your ethics committee or legal team that consent on this basis is suitable for your project.


Donation from within your organisation
Within certain research organisations and groups, it is not unusual for colleagues to donate blood to support internal research programmes. This route can be advantageous due to low costs and rapid delivery, but all aspects should be considered before going ahead with this supply option.
Supply times and consistency
Leveraging internal donors is cost effective and the time between blood draw and usage can be very short. However, depending on the size of your organisation and the willingness to volunteer, the donor pool can be very limited. The volume that can be collected is also limited due to collection processes used internally, which only allow for a small volume to be taken per donor. Therefore, depending on your application requirements and any future need to scale up, you might find that internal donation isn’t able to meet your needs.
Donor characteristics and lifestyle
As mentioned above, depending on the organisations size and willingness to donate, the diversity of your donor pool may be restricted. Therefore if your study requires several donors with specific characteristics, such as BMI, ethnicity or smoker status, then it is unlikely that you will be able to source all the samples through internal volunteer donors alone.
Ethical and consent requirements
Robust anonymisation
Using internal blood donors can raise some ethical considerations. For example, it is essential that you have a robust method to anonymise your samples before collecting internally, to ensure they cannot be traced back to individual colleagues. Once you have these systems in place, you would also need
to plan for the possibility that your research could uncover underlying health problems. In the worst cases, if samples are not properly anonymised then the wider team could discover a diagnosis which would raise confidentiality concerns.
Consent processes
Finally, labs using internal donors are more likely to have rudimentary consent processes in place, so if you do choose an internal supply, it is best to check your study is covered by their consent and that they have waived their IP rights.
Blood product formats available
Any blood product format can be generated from the blood drawn from internal volunteers, providing that you have access to the reagents, instrumentation and expertise required to process whole blood and to perform QC on the resulting samples. While most labs have these capabilities, these processing steps require an investment of time and resource which should also be considered.
Collection and processing
As collection is all in-house, you should have tighter control over blood collection and processing protocols. However, the ad- hoc approach of relying on internal donors means that this is not guaranteed. This could affect your experimental setup and have downstream repercussions, such as inconsistent results or unreliable data.
Specialist commercial blood collection suppliers
Scientists can now secure healthy blood samples from commercial organisations that specialise in the supply of fresh blood products for research use. Typically, these organisations can guarantee delivery on the same day or day after blood collection nationally, with more flexibility of collection and processing to better meet your needs.
Supply times and consistency
Finding a supplier that has a large pool of donors and can guarantee rapid delivery can help you avoid the pitfalls associated with aged blood products. Specialist suppliers have dedicated clinics for blood collection, so can better adhere to your timeframes and frequency requirements. This will mean you shouldn’t experience project delays as a result of samples not being available.
Donor characteristics and lifestyle
The large donor pools often recruited by specialist commercial suppliers also means that specific donor requests, such as age, ethnicity, blood group or whether they are medication-free can be better met. Sourcing a consistent supply of these samples can be a challenge, so specialist suppliers can be beneficial to researchers with precise requirements.
Ethical and consent requirements
Consent procedures are more robust when using a specialist commercial supplier, so you can be confident that your IP is protected and that you own any resulting data from donor samples. As these suppliers specialise in blood for research, donors are fully informed as to how their samples will be used and give explicit consent for their donation to be used for a wide range of applications, including commercial, genetic and animal-model research.
Blood product formats available
Specialist providers offer a wide range of products, including whole blood, leukopaks, PBMCs, immune cells, buffy coat, plasma, serum and red blood cells. Purchasing the format you require, rather than processing the raw samples yourself, can minimise delays in processing and save time and resources in house. Commercial suppliers also adhere to robust processing procedures, so you can be confident that the samples you receive will be consistent.
Collection & processing
Protocol flexibility
Sourcing fresh blood products is the primary purpose of these suppliers, so there is no restriction on collection or processing, as there may be with other supply options. Choosing a specialist supplier gives you the opportunity to customise the collection and processing protocols to meet your exact requirements.
Following best-practices
As specialists in blood collection for research, these organisations are well aware of best practises and should be able to guarantee processing within the recommended 8-hour time period.5 Some commercial specialists can even isolate PBMCs from blood samples within 5 hours of venepuncture, so you have peace of mind that there will be less variation between samples.
If you have a challenging research project, requiring specific samples and processing procedures, it is always worth getting a cost estimate from a specialist supplier that you can build into your project budget.
Securing the right source of fresh blood products for your needs
As we have explored, there are several options open to researchers looking to use fresh blood in their research. The right option for you will depend on the specific needs of your study.
In most cases, blood should arrive as fresh as possible after collection to ensure reliable results. If your research requires donors with specific characteristics or samples in a specific format, then it’s important to find a supplier that can consistently deliver against these requirements.
For scientists working in a commercial setting, it is imperative that products come with consent to cover your study, therefore we recommend building an internal process to cover this or select a supplier that offers this as part of their service.
Regardless of your application, to ensure you get the best possible results, it is important to work with a blood supplier you can trust to deliver the quality of products you need, when you need them.
To learn more about the specialist commercial solutions offered by the team at Research Donors, please get in contact with one of our distributors to discuss your project.
Authors
 James Reed
James Reed
James is the co-founder and Managing Director of Research Donors Ltd. With over 17 years’ experience in the public health sector, he has an in-depth understanding of the operational and strategic management of medicine, pathology, surgery, therapies and theatres.
As an HCPC state-registered Biomedical Scientist, James also has considerable experience in haematology and blood transfusion, and serves as a member of the NEQAS National Scientific Advisory Committee for blood cell morphology.
 Dr Vashu Pamnani
Dr Vashu Pamnani
Vashu is a Senior Business Manager for Human Blood Biospecimens Services. Studying at the Max Planck Institute for Biochemistry and Psychiatry in Germany, he gained his PhD focusing on novel ATPases in Archael bacteria in 1997.
Following this, Vashu undertook post-doctoral research at the Sealey Centre for DNA Repair at the University of Texas Medical Branch, USA, where he identified and isolated DNA repair mechanism proteins in yeast and humans. Vashu then went on to gain extensive experience of the commercial life science sector.
References
- Roche. FDA grants first liquid biopsy approval to the Roche cobas® EGFR mutation test v2. 01 Jun 2016. https://diagnostics.roche.com/us/ en/news-listing/2016/fda-grants-first-liquid-biopsy-approval-to-the-roche-cobas-egfr-mutation-test-v21.html (Accessed 26 June 2019).
- ISBER. Best practices: recommendations for repositories fourth edition. 2018. https://c.ymcdn.com/sites/isber.site-ym.com/resource/ resmgr/Best_Practices_4th_Edition/ISBER_Best_Practices_Recomme.pdf (Accessed 21 June 2019).
- Bull M, Lee D, Stucky J, et al. Defining blood processing parameters for optimal detection of cryopreserved antigen-specific responses for HIV vaccine trials. Journal of Immunological Methods. 2007. DOI: 10.1016/j.jim.2007.02.003
- Kong F-M, Zhao L, Wang L, Chen Y et al. Ensuring sample quality for blood biomarker studies in clinical trials: a multicentre international study for plasma and serum sample preparation. Translational lung cancer research. 2017. 6(6):625-634
- Hamot G, Ammerlaan W, Mathay C, et al. Method validation for automated isolation of viable peripheral blood mononuclear cells. Biopreservation and biobanking volume 13, number 3. 2015. DOI: 10.1089/bio.2014.0054.
- Betsou F, Lehmann S, Ashton G, et al. Standard preanalytical coding for biospecimens: defining the sample PREanalytical code. Cancer epidemiol biomarkers Prev. 2010. DOI 10.1158/1055-9965.
- McKenna K, Beatty K, Vicetti Miguel R, Bilonick R. Delayed processing of blood increases the frequency of activated CD11b+ CD15+ granulocytes which inhibit T cell function. Journal of Immunological Methods [Internet]. 2009. 341(1-2):68-75. Available from: https://www. ncbi.nlm.nih.gov/pubmed/19041316 (Accessed 3 June 2019).





